To take on the global pain epidemic, we need effective tools. Research shows when people learn about pain, their lives are improved. The best part? You can improve your outcomes without impacting the valuable time you have in the clinic.
Scroll to learn more
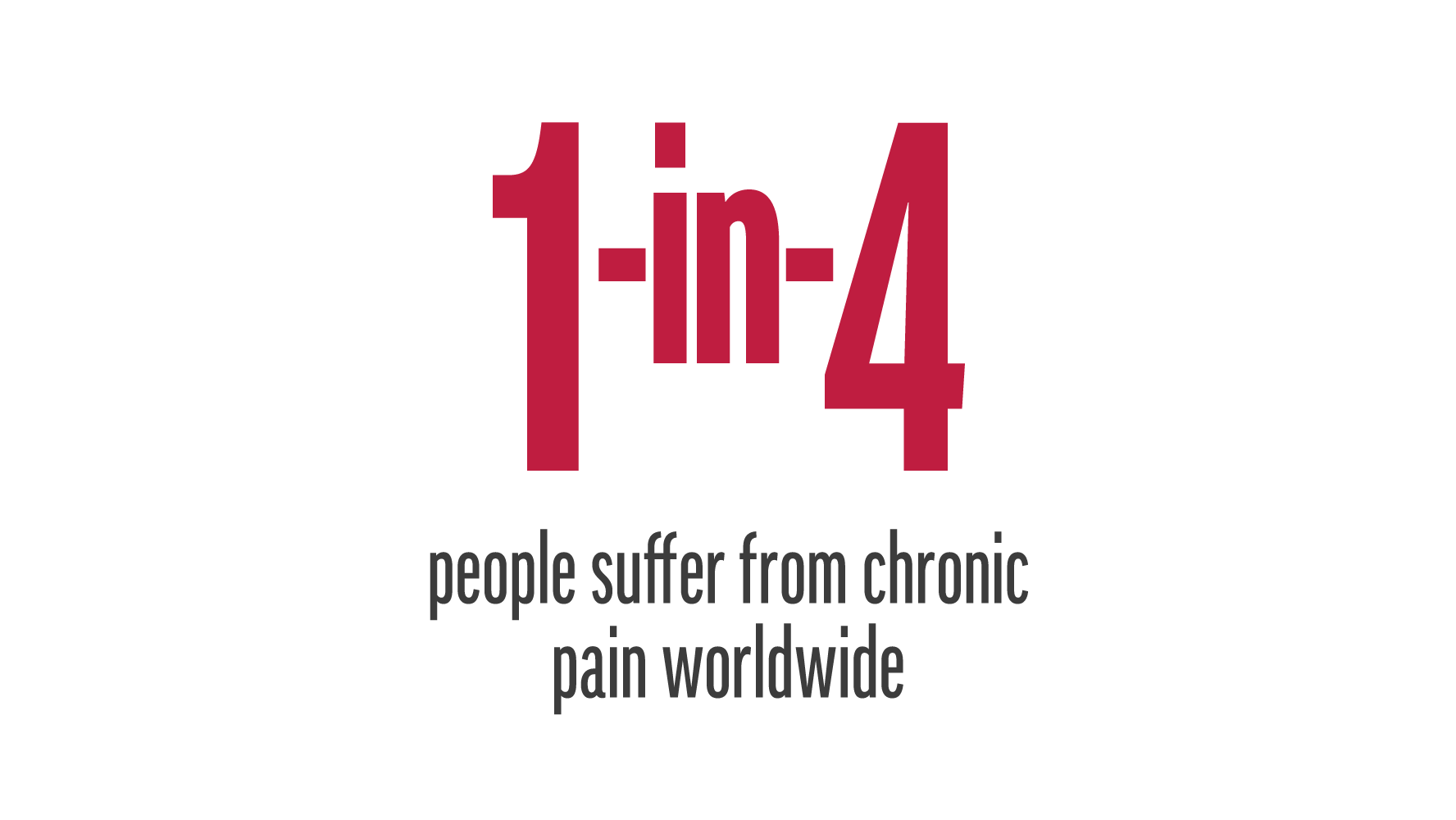
CHRONIC PAIN IS A GLOBAL EPIDEMIC


Reference:
- Global Burden of Disease Study C. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. Aug 22 2015;386(9995):743-800.
- Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81(9):646-656.
Reference
- Global Burden of Disease Study C. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. Aug 22 2015;386(9995):743-800.
- Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81(9):646-656.
Reference:
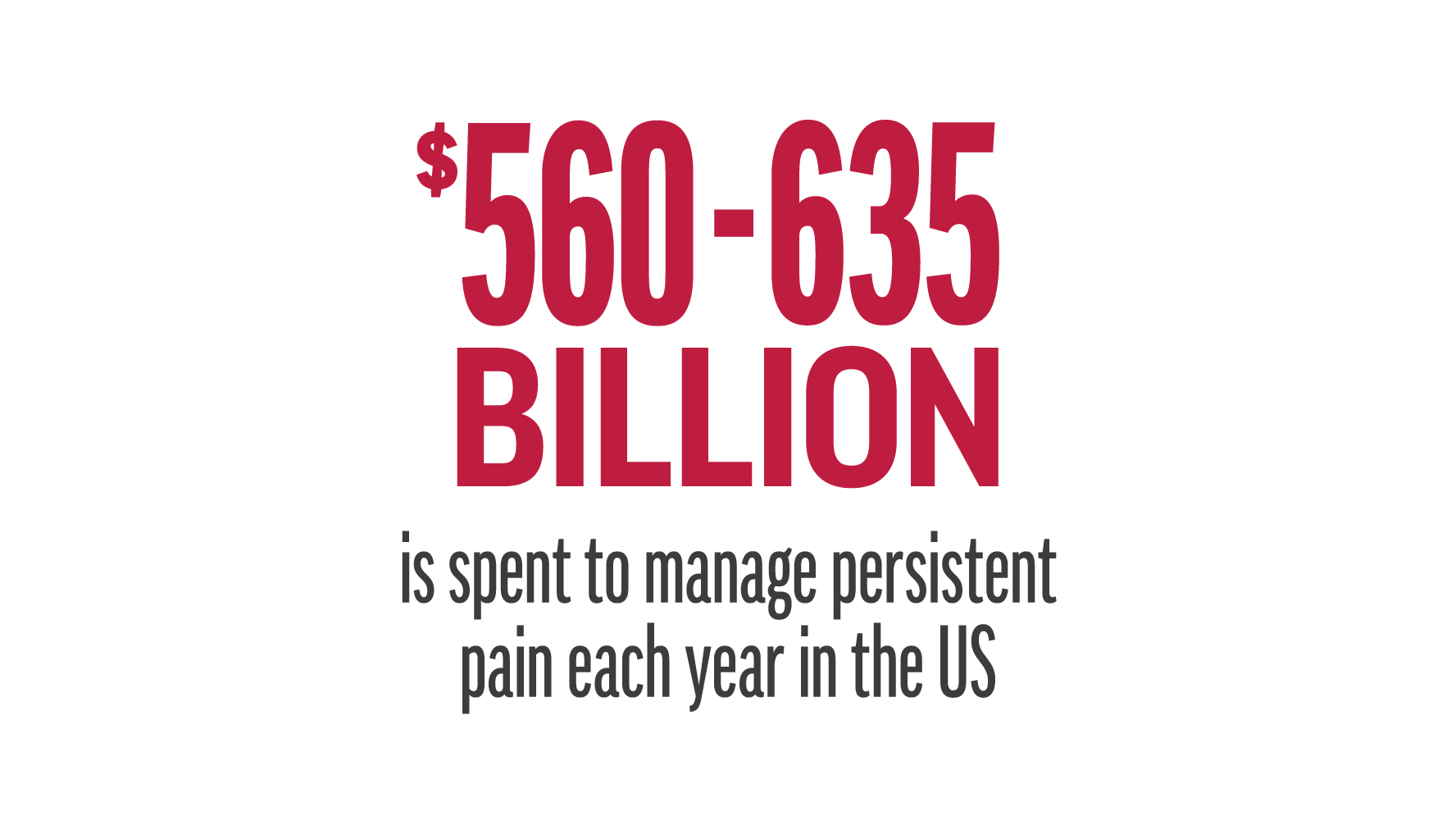
- Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: The National Academies Press; 2011.
Reference
- Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: The National Academies Press; 2011.
Reference:
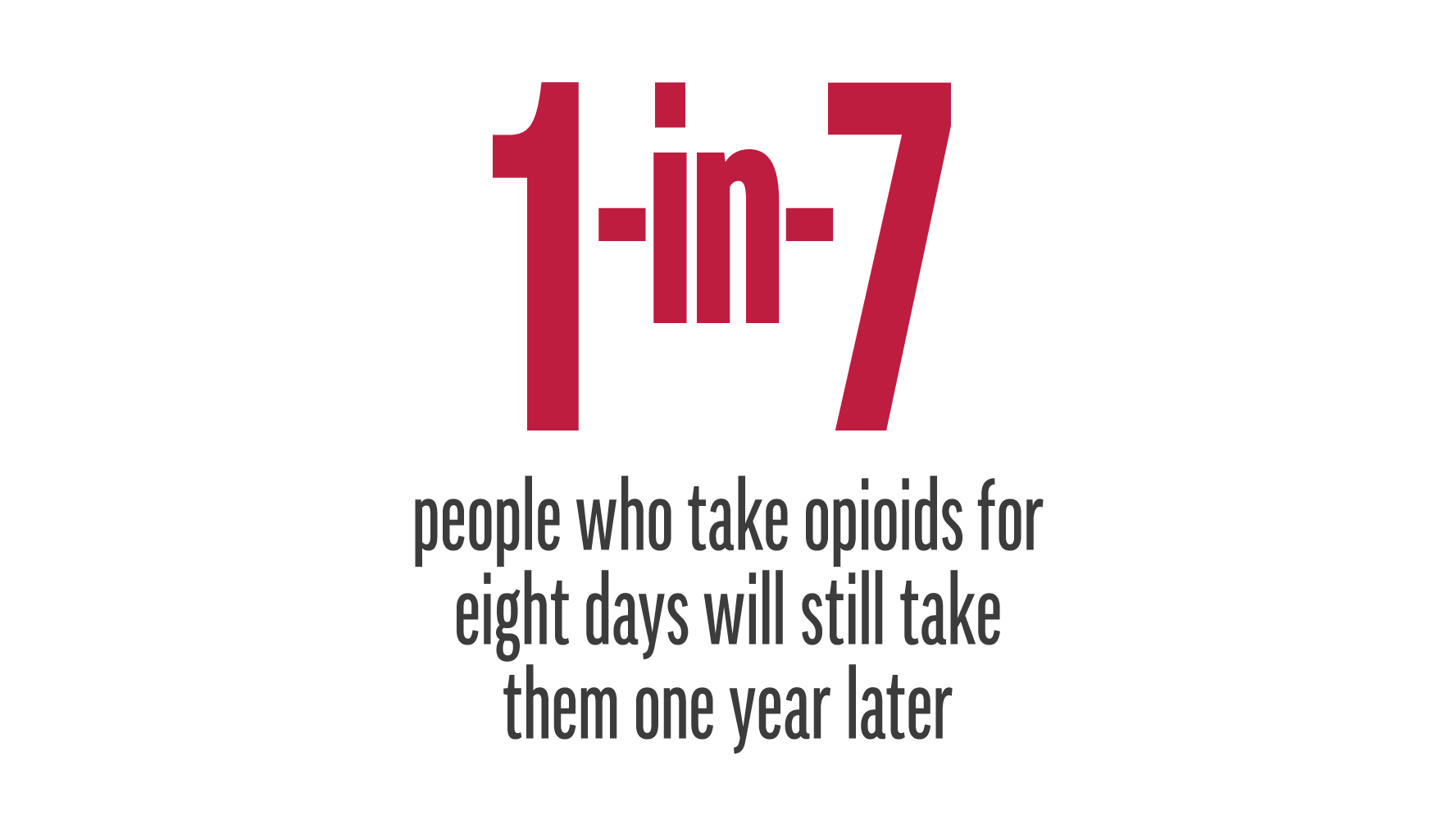
- 1 in 7 people will still take opioids one year later if they take opioids for 8 days.
- Shah, A., et al. (2017). Characteristics of Initial Prescription Episodes and Likelihood of Long-Term Opioid Use - United States, 2006-2015. MMWR Morb Mortal Wkly Rep 66(10): 265-269.
Reference
- 1 in 7 people will still take opioids one year later if they take opioids for 8 days.
- Shah, A., et al. (2017). Characteristics of Initial Prescription Episodes and Likelihood of Long-Term Opioid Use - United States, 2006-2015. MMWR Morb Mortal Wkly Rep 66(10): 265-269.
Reference:
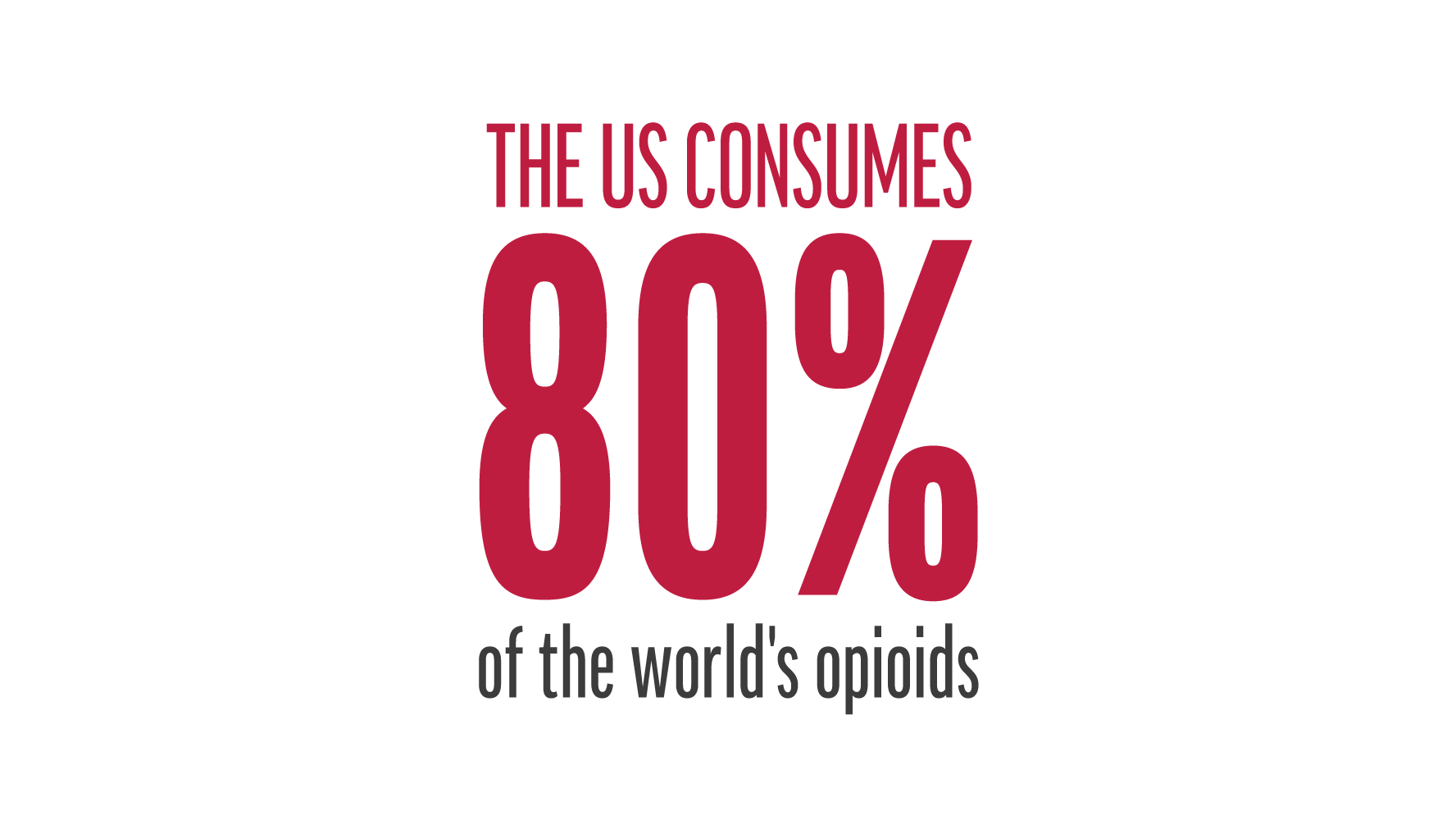
- Manchikanti, L., et al., Therapeutic use, abuse, and nonmedical use of opioids: a ten-year perspective. Pain physician, 2010. 13(5): p. 401-35.
Reference
- Manchikanti, L., et al., Therapeutic use, abuse, and nonmedical use of opioids: a ten-year perspective. Pain physician, 2010. 13(5): p. 401-35.
Reference:
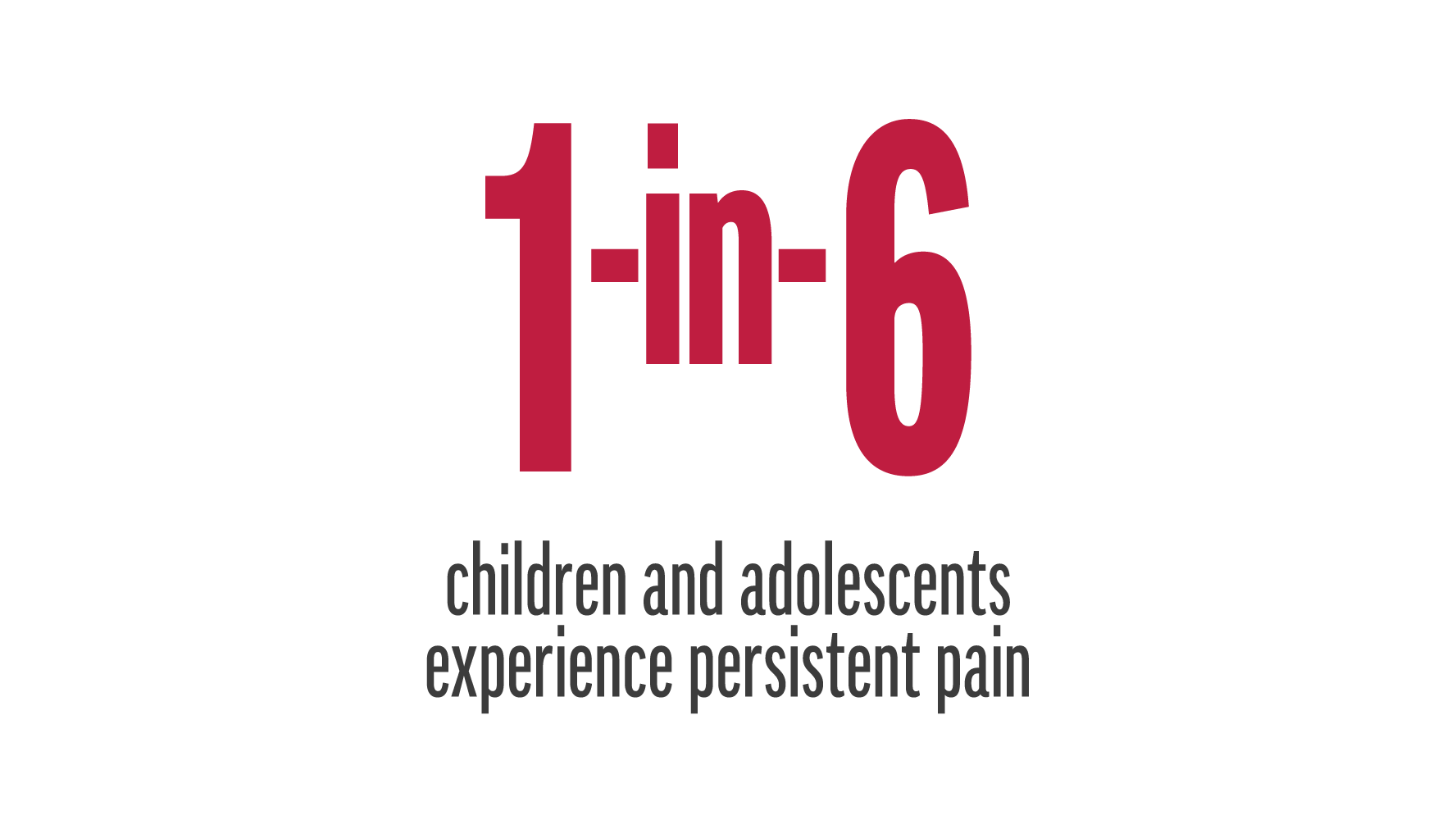
- Perquin CW, Hazebroek-Kampschreur AA, Hunfeld JA, et al. Pain in children and adolescents: a common experience. Pain. 2000;87(1):51-58.
Reference
- Perquin CW, Hazebroek-Kampschreur AA, Hunfeld JA, et al. Pain in children and adolescents: a common experience. Pain. 2000;87(1):51-58.
PNE IS PART OF THE SOLUTION


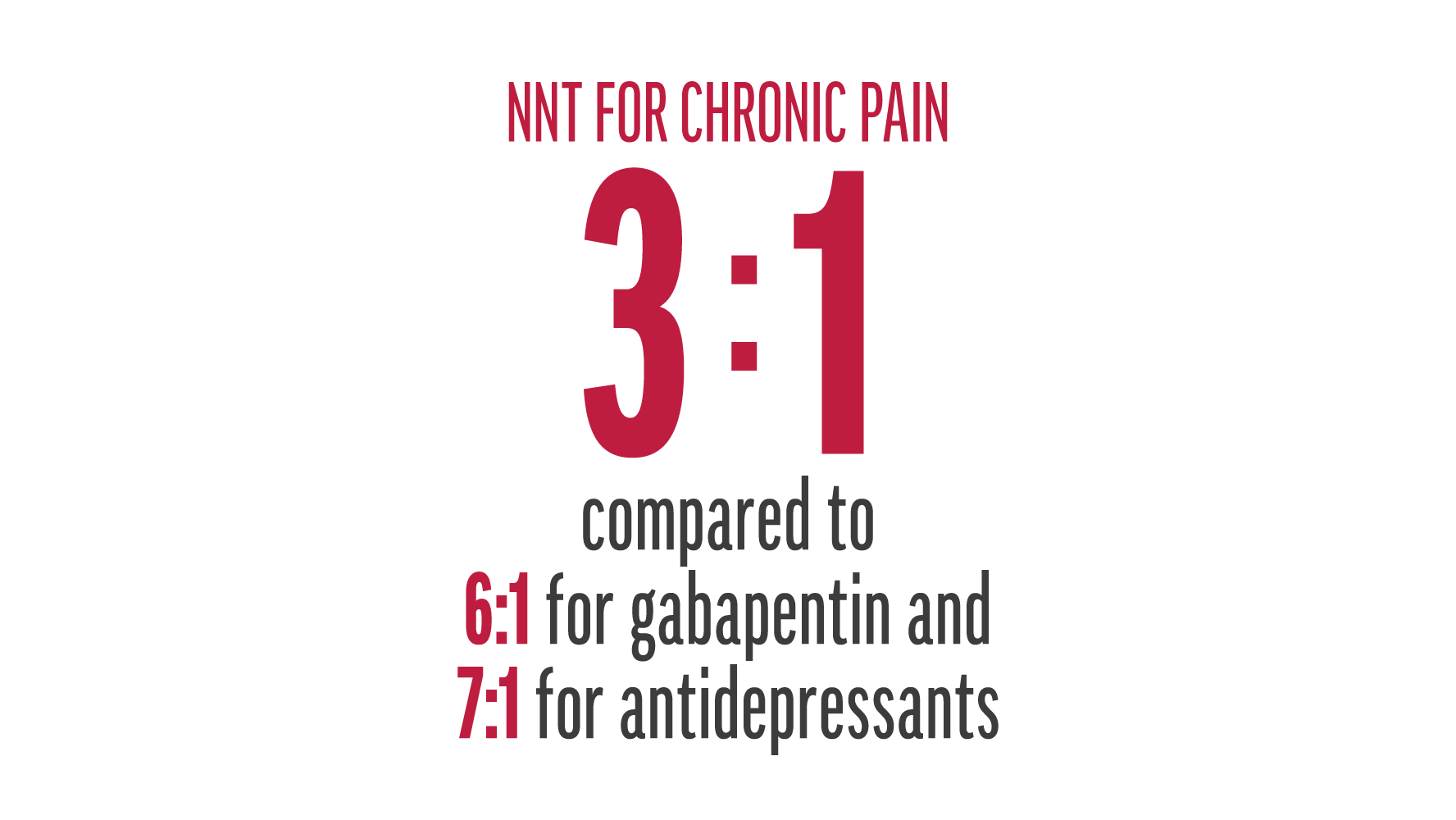
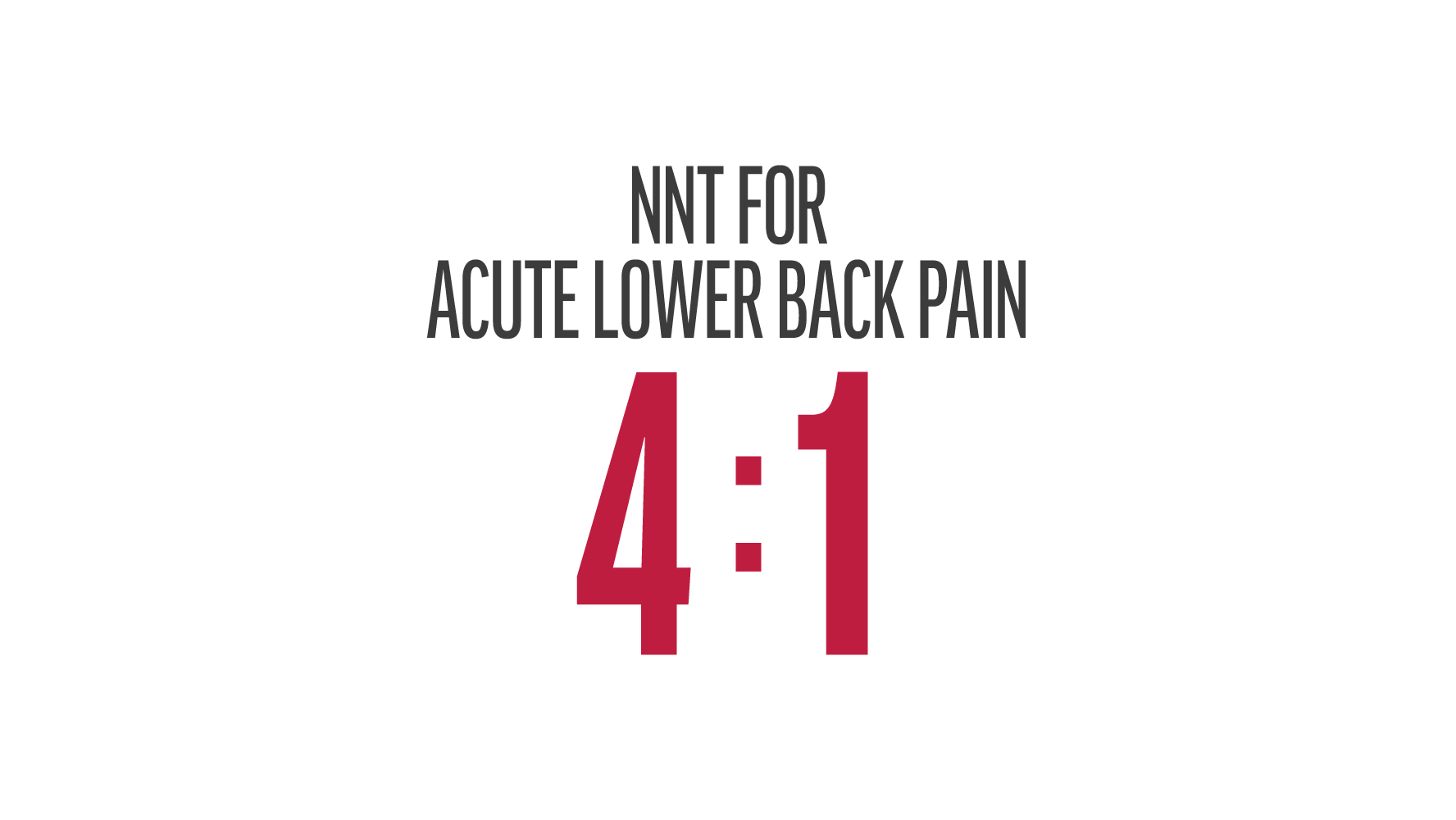
Reference:
- Moseley L. Combined physiotherapy and education is efficacious for chronic low back pain. Aust J Physiother. 2002;48(4):297-302.
- Moore RA, Wiffen PJ, Derry S, McQuay HJ. Gabapentin for chronic neuropathic pain and fibromyalgia in adults. The Cochrane database of systematic reviews. 2011(3):CD007938.
- Lynch ME, Watson CP. The pharmacotherapy of chronic pain: a review. Pain research & management. Spring 2006;11(1):11-38.
Reference
- Moseley L. Combined physiotherapy and education is efficacious for chronic low back pain. Aust J Physiother. 2002;48(4):297-302.
- Moore RA, Wiffen PJ, Derry S, McQuay HJ. Gabapentin for chronic neuropathic pain and fibromyalgia in adults. The Cochrane database of systematic reviews. 2011(3):CD007938.
- Lynch ME, Watson CP. The pharmacotherapy of chronic pain: a review. Pain research & management. Spring 2006;11(1):11-38.
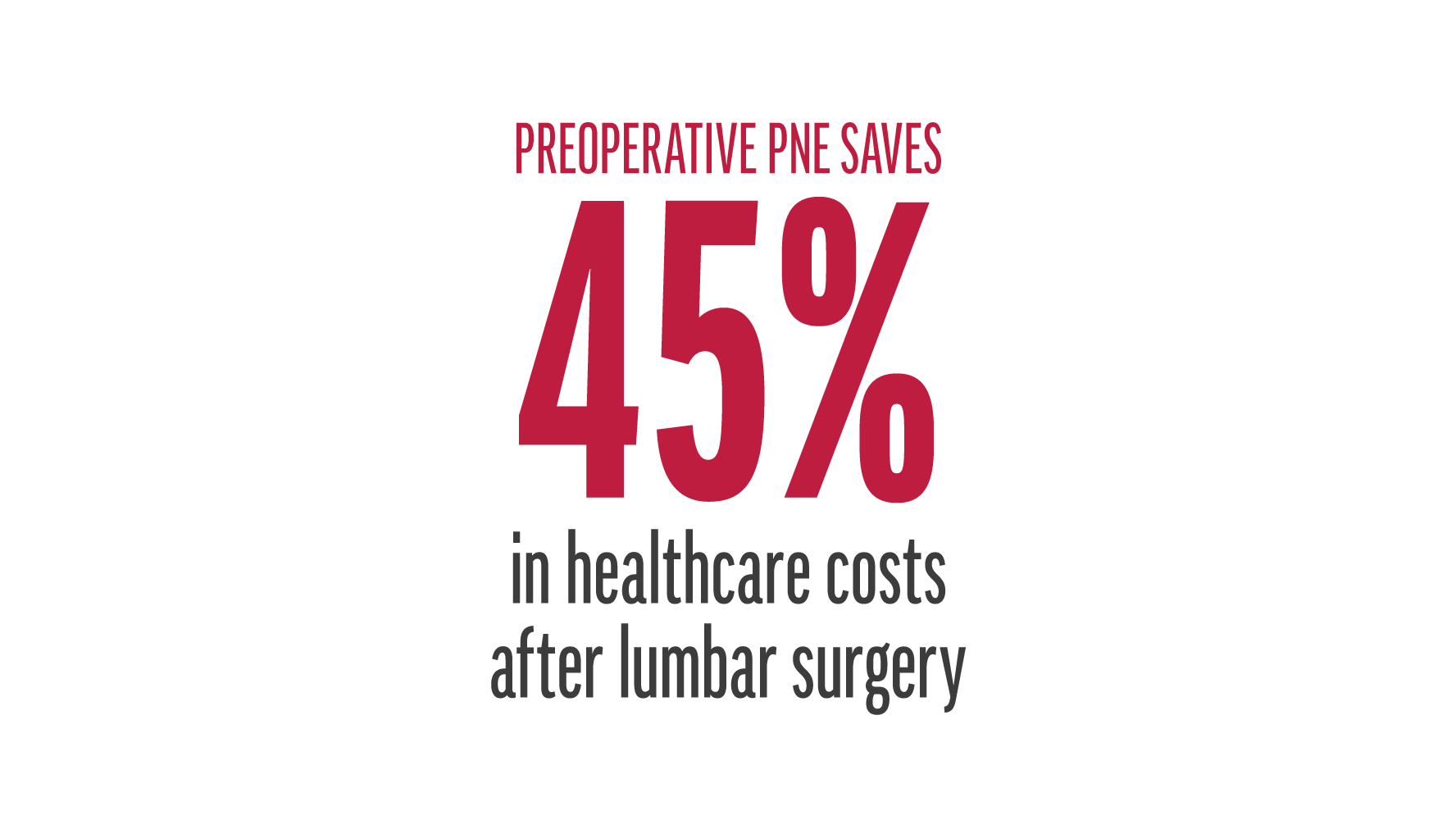
Reference:
- Louw A, Diener I, Landers MR, Puentedura EJ. Preoperative pain neuroscience education for lumbar radiculopathy: a multicenter randomized controlled trial with 1-year follow-up. Spine. Aug 15 2014;39(18):1449-1457.
Reference
- Louw A, Diener I, Landers MR, Puentedura EJ. Preoperative pain neuroscience education for lumbar radiculopathy: a multicenter randomized controlled trial with 1-year follow-up. Spine. Aug 15 2014;39(18):1449-1457.
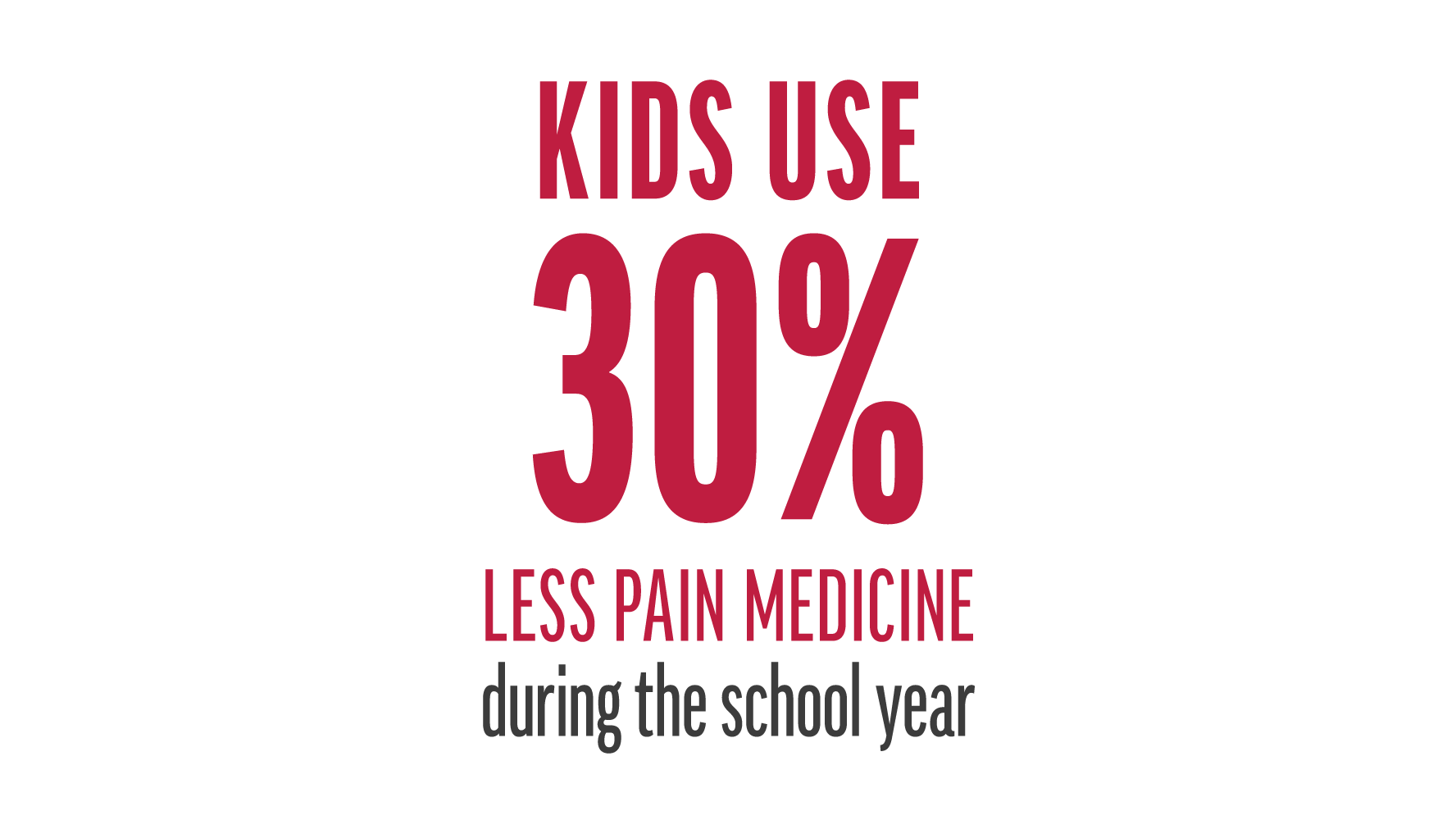
Reference:
- Louw, A., et al. (2020). "Behavior Change Following Pain Neuroscience Education in Middle Schools: A Public Health Trial." Int J Environ Res Public Health 17(12).
Reference
- Louw, A., et al. (2020). "Behavior Change Following Pain Neuroscience Education in Middle Schools: A Public Health Trial." Int J Environ Res Public Health 17(12).
Reference:
- Louw, A., et al. (2019). Immediate effect of pain neuroscience education for recent onset low back pain: an exploratory single arm trial. J Man Manip Ther: 1-10.
Reference
- Louw, A., et al. (2019). Immediate effect of pain neuroscience education for recent onset low back pain: an exploratory single arm trial. J Man Manip Ther: 1-10.
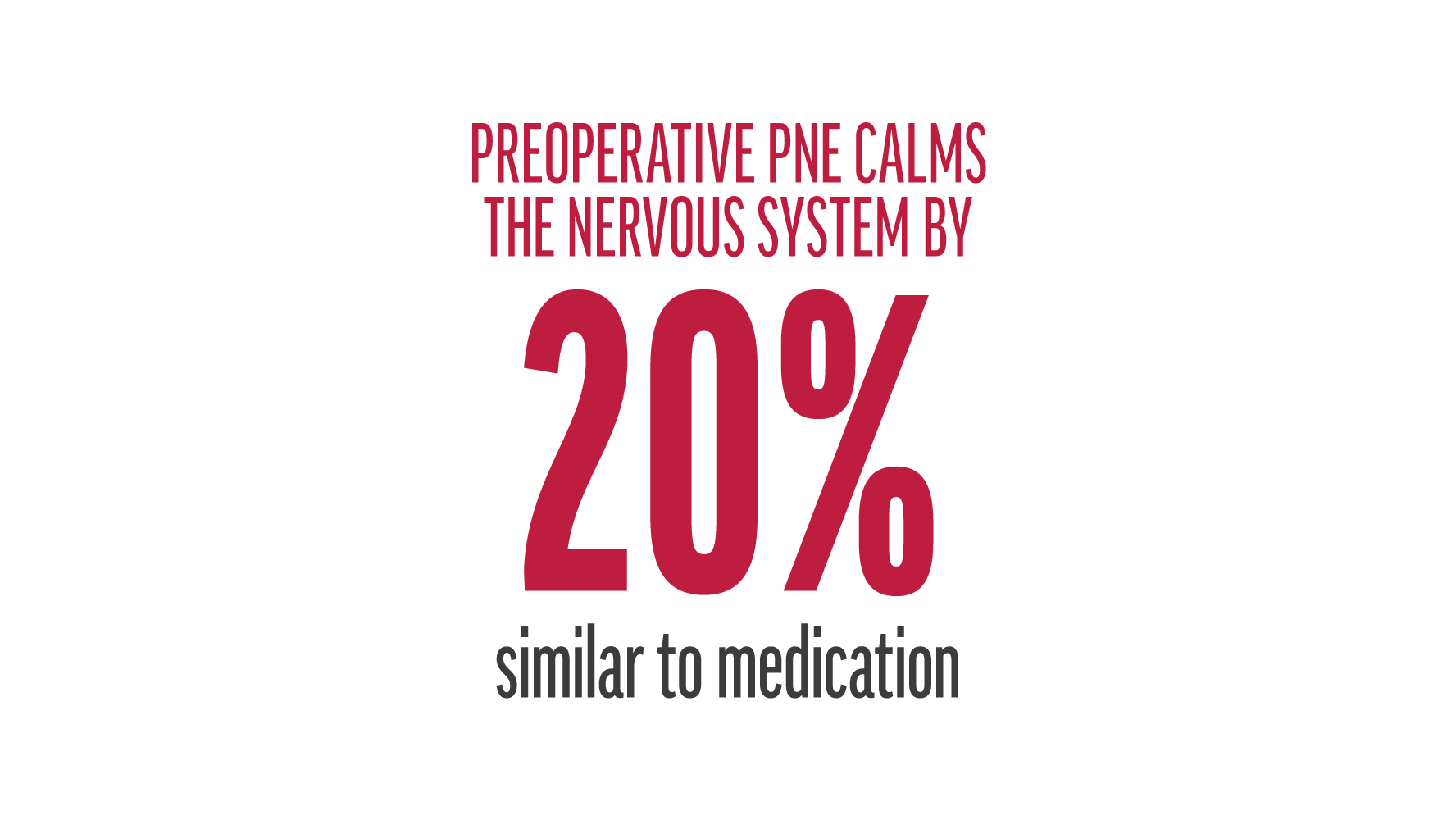
Reference:
- Louw, A., et al. (2018). Immediate preoperative outcomes of pain neuroscience education for patients undergoing total knee arthroplasty: A case series. Physiotherapy theory and practice: 1-11.
- Louw, A., et al. (2020). "Preoperative pain neuroscience education for shoulder surgery: A case series." S Afr J Physiother 76(1): 1417.
Reference
- Louw, A., et al. (2018). Immediate preoperative outcomes of pain neuroscience education for patients undergoing total knee arthroplasty: A case series. Physiotherapy theory and practice: 1-11.
- Louw, A., et al. (2020). "Preoperative pain neuroscience education for shoulder surgery: A case series." S Afr J Physiother 76(1): 1417.

